International FES Centre®
The International FES Centre® was established in 2018 and offers access to inpatients and outpatients for neurological and musculoskeletal rehabilitation.
FES at the Swiss Paraplegic Centre (SPC)
Treatment
In 1992, functional electrical stimulation (FES) has been introduced as a therapeutic intervention at the SPC and has been an integral component the rehabilitation of inpatients and outpatients ever since. All requirements specified within the general considerations of the International Functional Electrical Stimulation Society (IFESS) (Education – IFESS) are implemented in the rehabilitation of people with spinal cord injury and in neurorehabilitation in general.
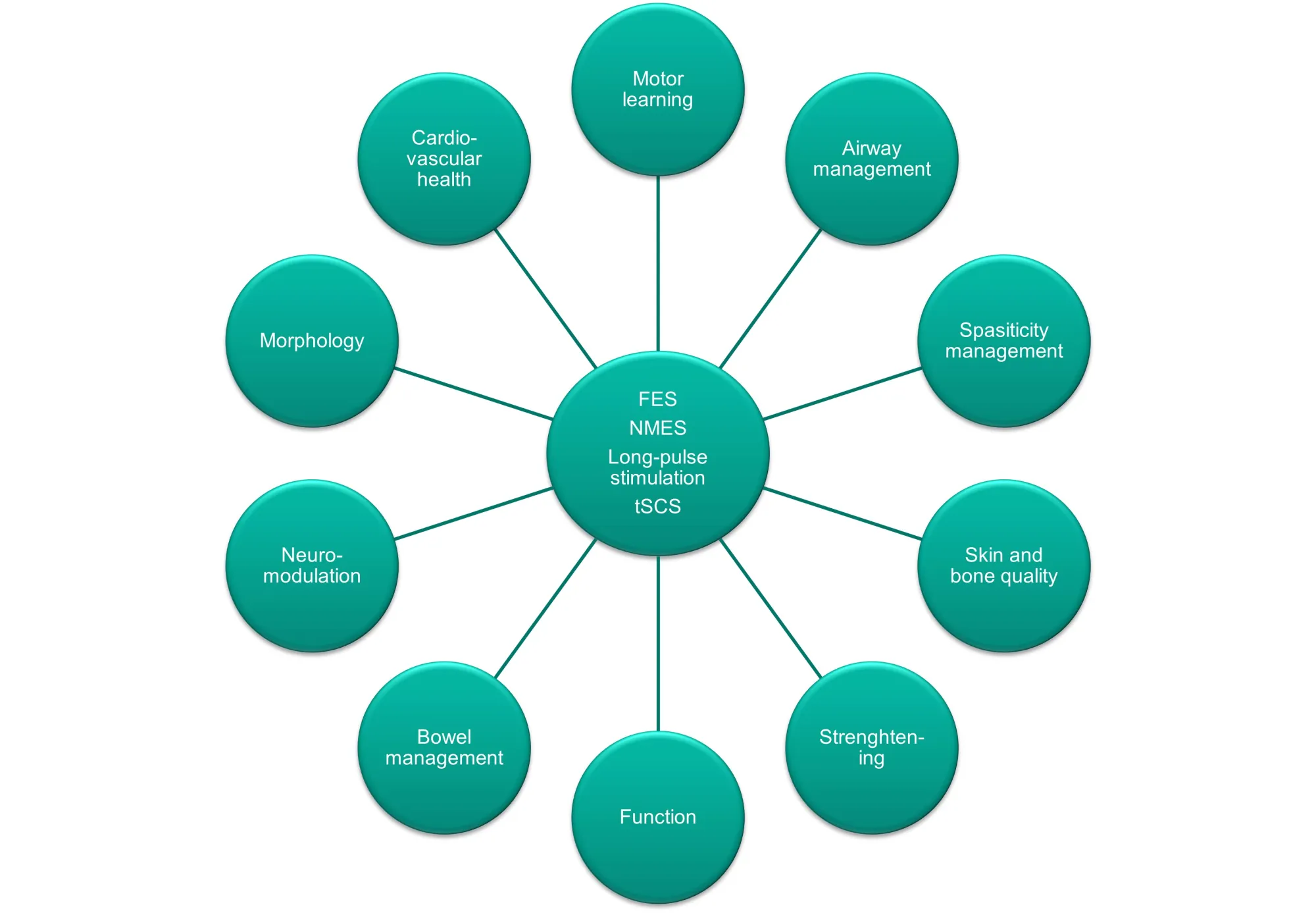
It comprises the integration of all up-to-date technologies in the domain of electrical stimulation. This implies the application of functional electrical stimulation (FES), neuromuscular electrical stimulation (NMES), direct muscle stimulation and cervical/lumbar transcutaneous spinal cord stimulation (tSCS).
The combined application of conventional physical and occupational therapy modalities, with or without the use of robotics, is carried out with simultaneous electrical stimulation according to the standards defined by the International Functional Electrical Stimulation Society (IFESS).
The following electrical stimulation treatment modalities are offered:
What does“functional electrical stimulation” mean?
Reference: Ines Bersch, Upper and Lower Motoneuron Lesions in Tetraplegia-Diagnostic and therapeutic Implications of Electrical Stimulation, ISBN 978-91-7833-408-7
FES is the treatment method which implies the application of electrical impulses instead of nerve stimuli to the muscle. It leads to the contraction of one or of multiple muscles. Electrical stimulation can help to establish a new functional balance, either by supporting or by replacing a certain function.
When using electrical stimulation, electrodes are placed on the skin and then used to create an electrical field. Under the influence of this To conduct the electrical stimulation, an artificial electrical field is created through the application of electrodes on the skin. The nerves and/or muscles underlying this electrical field are stimulated and the muscle will contract. The so-called muscle contraction that is being elicited through electrical stimulation is similar to a physiological (i.e. normal) muscle contraction.
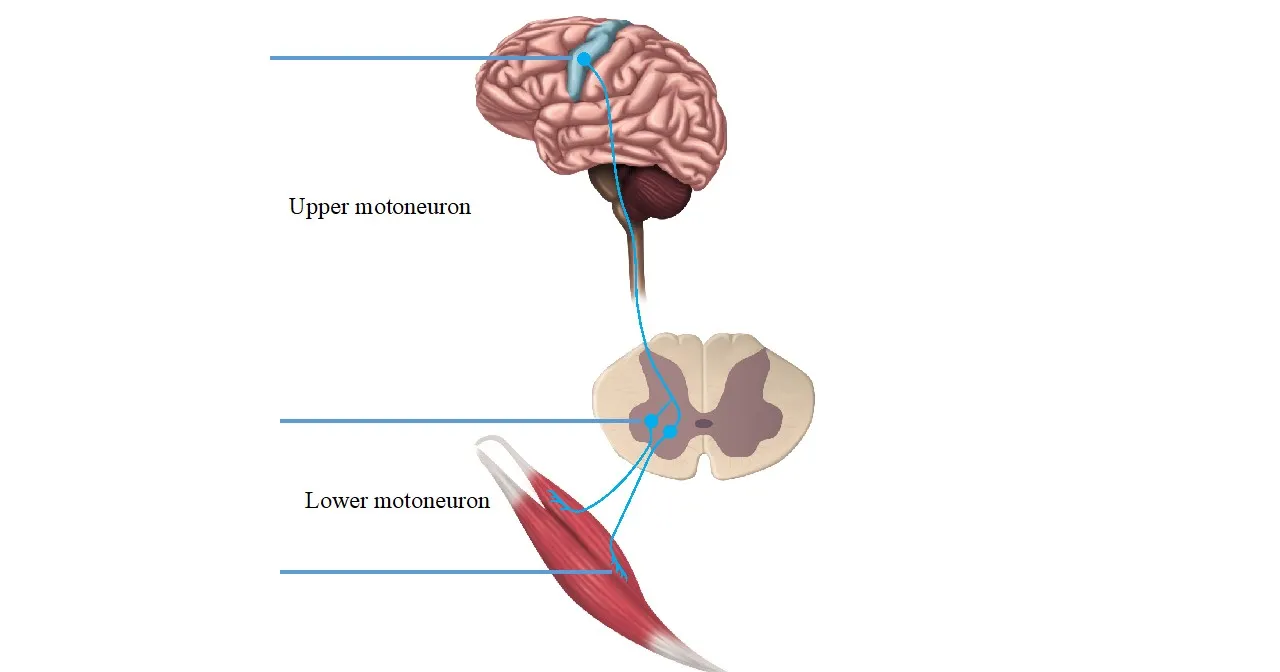
There exist two types of damages to the central nervous system: the damage to the upper motoneuron and the damage to the lower motoneuron.
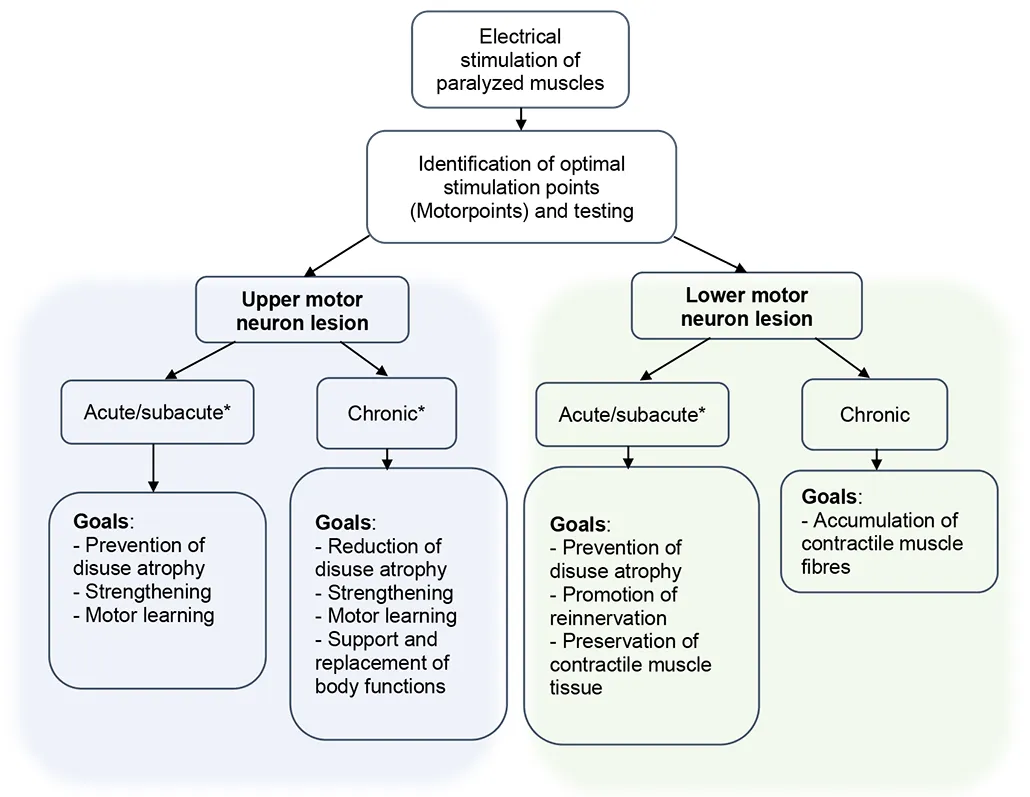
In people with a damaged upper motoneuron, the nerves below the level of the lesion are stimulated. In people with a lower motoneuron damage, the affected muscles are stimulated directly.
* acute/sub-acute £ 6 months; *chronic ³ 6 months after injury/disease
#acute/sub-acute £ 2 years; #chronic ³ 2 years after injury/disease
Reference: Ines Bersch. Upper and Lower Motoneuron Lesions in Tetraplegia - Diagnostic and Therapeutic Implications of Electrical Stimulation, ISBN 978-7833-408-7
Research
We conduct studies aiming to further improve the current body of evidence and prove the effectiveness of the method. In these clinically relevant studies, we investigate the effect of electrical stimulation regarding structural and functional changes in people with spinal cord injury and in individuals with neurological impairments. The objective is to demonstrate the relevance of the intervention and to implement it as a treatment standard in the long term. The uttermost goal is to improve the quality of life of people with spinal cord injury or of people living with a neurological disease and who are being restricted in their mobility or in their participation in social life.
Ongoing studies at the SPC
Education
We offer advanced training and educational courses. We organize a certified two-day course once a year, in which electrical stimulation and its application in the clinical/therapeutic field will be elaborated. The internationally advertised course takes place on the third Friday and Saturday in November. Beside the acquisition of knowledge regarding theoretical concepts and learning practical skills, the course offers an opportunity for international and interprofessional exchange.
Furthermore, we offer webinars taking place in the early evening. Their aim is to provide “learning snacks” regarding various topics involving the application of FES, NMES, direct muscle stimulation and tSCS.
We also accept advanced training or education inquiries from external private practices and hospitals. To this end, we kindly ask you to mention a specific topic within your request so that we can tailor an individualized program that concurs with your needs and wishes. These trainings can be conducted in an online, in-person or in a hybrid format.
Inpatient care
Inpatient treatment involving FES is guaranteed through the therapist in charge. They are supervised by both FES-specialists and therapy experts. A continuative treatment in the International FES Centre® and a lifelong follow-up care are guaranteed.
Outpatient care
Treatment upon outpatient referrals including follow-up evaluations of people with spinal cord injury and/or with limitations of body functions due to damage to the spinal cord, such as reduced muscle strength, reduced sensibility, problems regarding bladder or bowel control and other neurological symptoms.
Upon outpatient referral to the International FES Centre®, all possibilities in respect to the application of electrical stimulation will be evaluated (i.e. FES, NMES or direct muscle stimulation, tSCS).
Furthermore, it is possible for outpatients to pursue treatment supported by physical and occupational therapists from different departments allowing to combine and integrate methods and technologies that rely on all kinds of electrical stimulation (e.g.: foot drop systems, stimulation devices for arm and/or hand making use of array electrodes).
We provide follow-up care with electrical stimulation of inpatients after their discharge upon receival of an appropriate prescription. Moreover, treatment is offered upon medical prescription, as a private service or in the form of a subscription.
Since 2022, we offer outpatient rehabilitation for national and international clients which involves physical and occupational therapy in combination with the appropriate electrical stimulation modality. Therapy can be conducted following agreement of health insurance coverage or through self-financing.
Moreover, patients from abroad have the possibility to receive an individual consultation at the International FES Centre® in order to investigate the different possibilities (see above) to implement electrical stimulation as a treatment modality. This 3-hour consultation comprises diagnostics, treatment and the testing of different stimulation devices and systems.
FES services / treatment methods
FES represents a multifaceted treatment method that is ideally combined with occupational therapy and/or physiotherapy. The stimulation programmes and relevant parameters should, however, be selected on a case-by-case basis. As a rule, the use of standard programmes has not provided promising results.
Structure
Links
Literature
Our specialists

Dr. Ines Bersch-Porada

Dr. med. Michael Baumberger

Dr. med. Urs Sonntag

Ursula Gföller

Susanne Opel

Charlene Eggenschwiler

Marie Alberty

Kathrin Schafer

Snjezana Tarac

Dr. med. Ulf Bersch
Contact

Administration FES Centre
Administration office hours
Monday, Tuesday, Thursday, Friday:
8 am to midday
1.30 pm to 4 pm
Wednesday:
Closed
Werden Sie jetzt Mitglied und erhalten Sie im Ernstfall 250 000 Franken.
Spenden Sie jetzt und unterstützen Sie unsere Projekte zugunsten von Querschnittgelähmten.